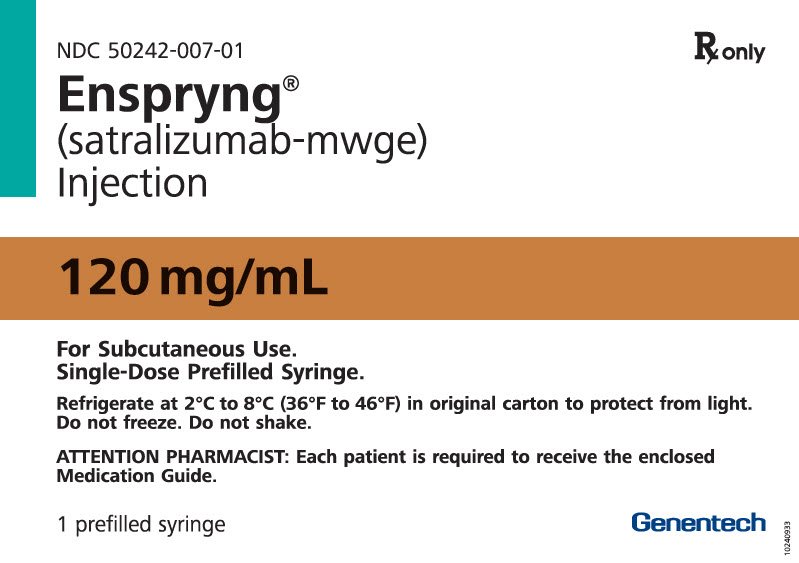
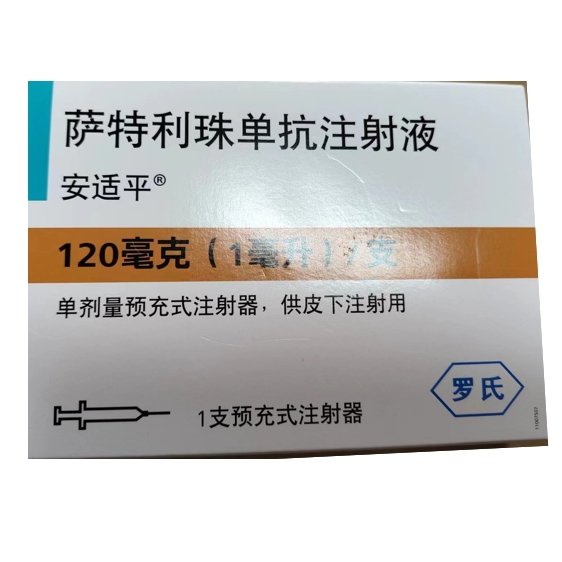
安适平®;Enspryng®. 英文名称:Satralizumab Injection.
Function and indication: This product is used to treat neuromyelitis optica spectrum disorder (NMOSD) in adolescents aged ≥12 years (see [Children’s Use]) and adult patients with positive aquaporin 4 (AQP4) antibodies.
Dosage and Administration:
Evaluation before the first dose of Satlizumab Hepatitis B virus screening Hepatitis B virus (HBV) screening should be performed before starting this product. This product is contraindicated in patients with active HBV confirmed by positive surface antigen [HBsAg] and anti-HBV test results. For HBsAg-negative, hepatitis B core antibody-positive [HBcAb+] or HBV carriers [HBsAg+], please consult a liver disease specialist before and during treatment with this product (see [Contraindications] and [Precautions]). Tuberculosis screening Before starting treatment with this product, active tuberculosis should be evaluated and latent infection should be tested. For patients with active tuberculosis or tuberculosis screening who have no history of appropriate treatment, an infectious disease specialist should be consulted before starting treatment with this product (see [Contraindications] and [Precautions]). Liver transaminase screening Before starting treatment with this product, liver transaminases and serum bilirubin should be assessed (see [Precautions]). This product should be used with caution in patients with aspartate aminotransferase (AST) or alanine aminotransferase (ALT) levels above 1.5 times the upper limit of normal (ULN). Vaccination Since live attenuated or live vaccines are not recommended during treatment with this product, all live or live attenuated vaccines should be completed according to immunization guidelines at least 4 weeks before starting this product, and all inactivated vaccines should be completed at least 2 weeks before starting this product as much as possible (see [Precautions]). The recommended dose is for subcutaneous administration only. Before each use of this product, if active infection (including local infection) is suspected, it is recommended that patients consult a professional healthcare professional (HCP). If active infection exists, patients should delay the use of this product until the infection is controlled (see [Precautions]). The recommended loading dose of this product is 120 mg for the first three subcutaneous injections at weeks 0, 2, and 4, followed by a maintenance dose of 120 mg every 4 weeks. Delayed or Missed Doses If a dose is missed for any reason other than elevated liver enzymes, make up the missed dose as described in Table 1. Table 1 Recommended Doses for Delayed or Missed Doses Recommended Doses for Last Delayed or Missed Doses Maintenance Period Less than 8 Weeks or Missed Loading Dose Administer 120 mg subcutaneously as soon as possible, without waiting for the next scheduled dose. After a dose is delayed or missed during the maintenance period, reset the dosing schedule to every 4 weeks. Loading Period If the second loading dose is delayed or missed, administer as soon as possible, and give the third (and final) loading dose 2 weeks later. If the third loading dose is delayed or missed, administer as soon as possible, and give the first maintenance dose 4 weeks later. ≥8 Weeks to <12 Weeks Administer 120 mg subcutaneously at Weeks 0* and 2, followed by 120 mg subcutaneously every 4 weeks. ≥12 Weeks Administer 120 mg subcutaneously at Weeks 0*, 2, and 4, followed by 120 mg subcutaneously every 4 weeks. *“Week 0” refers to the first dose after a missed dose. Important Administration Instructions: This product should be administered by self-administration of subcutaneous injection by the patient under the guidance of the HCP. After appropriate training in subcutaneous injection technique, patients may self-administer or have their caregiver administer satelizumab if the HCP deems it appropriate. If the patient develops symptoms of a severe allergic reaction, they should seek medical attention immediately and should not be re-administered until evaluated by the HCP (see Contraindications and Precautions). Before use, remove the prefilled syringe from the refrigerator and place it outside the packaging at room temperature for 30 minutes. Do not warm this product in any other way. Visually inspect the solution for insoluble particles and discoloration before administration. Satelizumab injection should be a clear, colorless to light yellow liquid. Do not use if the solution is turbid, discolored, or has particles, or if any part of the prefilled syringe appears damaged. Instruct the patient to inject the entire dose (1 mL) in the syringe, which contains 120 mg of satelizumab. Inject this product subcutaneously in the abdomen or thigh. Rotate the injection site for each dose. Do not choose sites with moles, scars, or tender, abraded, red, hard, or broken skin for injection. Safety Monitoring During Treatment Abnormal liver enzymes ALT and AST levels should be monitored every 4 weeks during the first 3 months of treatment with this product, then every 3 months for one year, and then monitored as clinically indicated (see [Precautions]). If ALT or AST increases to more than 5 times the ULN, discontinue this product as follows: l If accompanied by an increase in bilirubin, discontinue this product and it is not recommended to restart this product. l If there is no increase in bilirubin above the ULN, when ALT or AST levels return to the normal range and the patient has been evaluated for benefit-risk, treatment with this product can be restarted according to the regimen in Table 2. Table 2 Recommended doses for restarting treatment after elevation of liver transaminases Last dose Recommended dose for restarting treatment <12 weeks Restart subcutaneous injection at 120 mg once every 4 weeks. ≥12 weeks Restart subcutaneous injection at 120 mg at weeks 0*, 2, and 4, and then at 120 mg every 4 weeks. *“0 weeks” refers to the time of the first dose after a missed dose. If treatment is restarted, liver parameters must be closely monitored, and if ALT/AST and/or bilirubin are subsequently observed to be above ULN, this product should be discontinued and it is not recommended to restart treatment again. Neutrophil count Monitor neutrophils for 4-8 weeks after starting treatment, and then monitor at regular intervals determined by the clinic. If the neutrophil count is less than 1.0×109/L and is confirmed by repeated testing, treatment with this product should be interrupted until the neutrophil count is >1.0×109/L (see [Precautions]).
Adverse reactions:
Clinical trials of adult patients with NMOSD who are positive for AQP4 antibodies Because clinical studies are conducted under a variety of different conditions, it is not possible to directly compare the incidence of adverse reactions observed in the clinical studies of a drug with the incidence of adverse reactions observed in the clinical studies of another drug, and may not reflect the incidence of adverse reactions observed in clinical practice. The safety of satelizumab was evaluated in two randomized, placebo-controlled clinical trials (Study 1 evaluated satelizumab without concomitant immunosuppressive therapy (IST) and Study 2 evaluated satelizumab with concomitant IST). Study 1 enrolled 41 patients with AQP4 antibody-positive disease who were treated with satelizumab, and Study 2 enrolled 26 patients with AQP4 antibody-positive disease who were treated with satelizumab (see Clinical Trials). During the double-blind, controlled treatment period, the median duration of exposure to satelizumab was approximately 2 years in Study 1 and 3 years in Study 2. The median duration of exposure to placebo was approximately 1 year in Study 1 and Study 2. Adverse reactions occurring in >5% of patients treated with satelizumab and at a higher incidence than in patients receiving placebo in Study 1 and Study 2 are shown in Tables 3 and 4, respectively. The most common adverse reactions (incidence ≥15% in the satelizumab-treated group in either study) were nasopharyngitis, headache, upper respiratory tract infection, gastritis, rash, arthralgia, pain in extremity, fatigue, and nausea. Table 3 Adverse Reactions Occurring in ≥4 satelizumab-treated patients in Study 1 and at a Rate Greater Than Placebo Adverse Reactions Satelizumab (N=41)% Placebo (N=23)% Rash Arthralgia Pain in extremity Fatigue Nausea Nasopharyngitis Pruritus Depression Cellulitis Neutropenia Increased creatine phosphokinase in blood Falls Table 4 Adverse Reactions Occurring in ≥3 satelizumab-treated patients in Study 2 and at a Rate Greater Than Placebo Adverse Reactions Satelizumab + IST (N=26)% Placebo + IST (N=26)% Nasopharyngitis Headache Upper respiratory tract infection Gastritis Arthralgia Pharyngitis Injection-Related Reactions In Study 1 and Study 2, injection-related reactions were reported in 9% of patients treated with satelizumab and in 8% of patients treated with placebo. In patients treated with satelizumab, these reactions were primarily mild to moderate in severity, and most occurred within 24 hours of injection. The most commonly reported systemic symptom was diarrhea. Local injection site reactions reported were pruritus, injection site reactions, and skin masses. Infections In Study 1, the infection rate was 51 patients per 100 patient-years (95% CI: 32,78) in patients treated with satelizumab compared to 108 patients per 100 patient-years (95% CI: 52,199) in patients receiving placebo. The incidence of serious infections was 5 patients per 100 patient-years (95% CI: 1,14) in patients treated with satelizumab compared to 4 patients per 100 patient-years (95% CI: 0,21) in patients receiving placebo. In Study 2, the infection rate was 168 patients/100 patient-years (95% CI: 100,265) in patients treated with satelizumab and 143 patients/100 patient-years (95% CI: 83,229) in patients treated with placebo. The incidence of serious infections was 4 patients/100 patient-years (95% CI: 1,15) in patients treated with satelizumab and 10 patients/100 patient-years (95% CI: 2,28) in patients treated with placebo. Laboratory Abnormalities Neutrophil Count Decreased In Study 1, neutrophil counts <1×109/L were observed in 10% of patients treated with satelizumab and 9% of patients treated with placebo. In Study 2, neutrophil counts <1×109/L were observed in 15% of patients treated with satelizumab and 4% of patients treated with placebo. In Study 1, one patient treated with satelizumab experienced a neutrophil count <0.5 × 109/L, and in Study 2, one patient discontinued satelizumab due to neutropenia. Decreased Platelet Count In Study 1, 26% of satelizumab-treated patients experienced a change in platelet count from normal at baseline to below the lower limit of normal (LLN) compared with 5% of patients receiving placebo. In Study 2, 35% of satelizumab-treated patients experienced a change in platelet count from normal at baseline to below LLN compared with 17% of patients receiving placebo. No patients experienced a decrease in platelet count to <50 × 109/L. Elevated Liver Enzymes In Study 1, 43% and 25% of satelizumab-treated patients experienced a change in ALT or AST from normal at baseline to above ULN, respectively, compared with 13% and 9% of patients receiving placebo. In Study 2, ALT or AST changes from normal baseline to above ULN occurred in 8% and 8% of patients treated with satelizumab, respectively, compared with 12% and 19% of patients treated with placebo, respectively. Combining Studies 1 and 2, 3% of patients treated with satelizumab experienced an increase in ALT or AST to >3×ULN, compared with no patients treated with placebo. These liver enzyme elevations were not associated with increases in total bilirubin. In Study 2, an ALT increase to >5×ULN was observed in one patient treated with satelizumab 4 weeks after the start of treatment, which returned to normal levels 78 days after the discontinuation of satelizumab. Dyslipidemia In Study 1 and Study 2, total cholesterol increases to >7.75 mmol/L (300 mg/dl) occurred in 12% and 15% of patients treated with satelizumab, respectively, compared with no patients treated with placebo. In Study 1 and Study 2, an increase in triglycerides to >3.42 mmol/L (300 mg/dL) occurred in 27% and 12% of patients treated with satelizumab, respectively, compared with 13% and 8% of patients receiving placebo, respectively.Fibrinogen LevelsIn Study 1, the median percent decrease in fibrinogen was 38% in patients treated with satelizumab and 5% in patients receiving placebo.In Study 2, the median percent decrease in fibrinogen was 33% in patients treated with satelizumab and 0% in patients receiving placebo.Complement LevelsIn Study 1, the median percent decreases in complement C3 and C4 levels were 23% and 50% in patients treated with satelizumab, respectively, compared with 0% and 1% in patients receiving placebo.In Study 2, the median percent decreases in complement C3 and C4 levels were 20% and 53% in patients treated with satelizumab, respectively, compared with 0% and 1% in patients receiving placebo. Weight Combining Study 1 and Study 2, 30% of patients treated with satelizumab experienced an increase in body weight of at least 7% from baseline compared with 8% of patients receiving placebo. 6% of patients treated with satelizumab experienced an increase in body weight of at least 15% from baseline compared with 4% of patients receiving placebo. Immunogenicity As with all therapeutic proteins, satelizumab may be immunogenic. Detection of antibody production is highly dependent on the sensitivity and specificity of the assay. In addition, the observed incidence of antibodies (including neutralizing antibodies) in an assay may be influenced by a variety of factors, such as assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. Therefore, comparisons of anti-satelizumab antibody rates in the studies described below with rates in other studies or other formulations may be misleading. Antidrug antibodies (ADA) were observed in 73% and 38% of patients receiving satelizumab during the double-blind period of Study 1 and Study 2, respectively. The ability of these ADA to neutralize satelizumab binding is unknown. Patients with greater body weight and lower exposure were more likely to develop ADA (regardless of IST treatment). Exposure was lower in ADA-positive patients. Although the development of anti-satelizumab antibodies was not found to affect the efficacy of satelizumab in these patients, the available data are too limited to draw definitive conclusions. Immunogenicity had no clinically relevant impact on safety. Based on the available information, neither dosing interruption nor dose adjustment is required for patients who develop ADA. Adolescent patients: Study 2 enrolled 7 adolescent patients in the double-blind period. During the double-blind period, 2 of the 3 patients who received placebo reported 7 adverse events. 3 of the 4 patients who received satelizumab reported 21 adverse events. The adverse events reported were different among the 7 patients. All adverse events were mild, no serious adverse events were reported, and all adverse events resolved or improved. Adverse events reported more than once were injection-related reactions, headache, dizziness, rhinitis, and decreased serum ferritin, of which only injection-related reactions were assessed by the investigator as being related to the study drug. No adolescent patient withdrew from study treatment due to adverse events.
Contraindications:
This product is contraindicated in the following patients: l Known hypersensitivity to satelizumab or any inactive ingredients (see [Precautions]). l Active hepatitis B infection (see [Precautions]). l Active or untreated latent
Share:
Products
Our offers
Health Classification
Let us work together to protect precious health