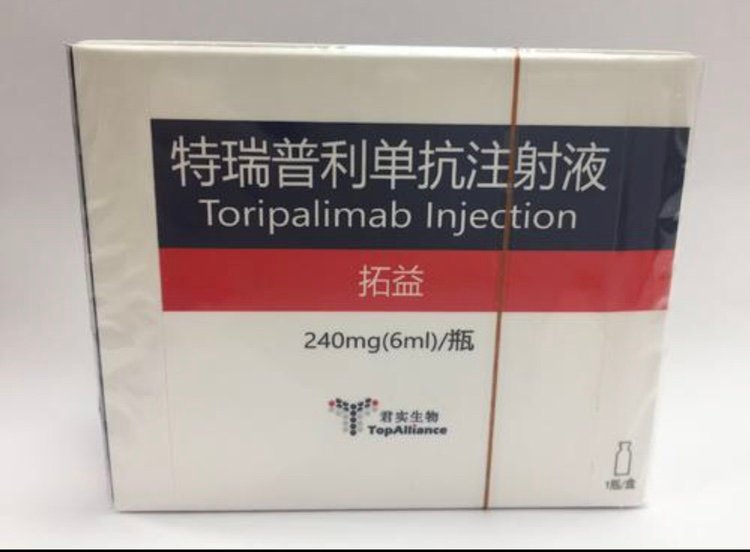
Toripalimab Injection.
Function and indication:
Toripalimab is indicated for the treatment of unresectable or metastatic melanoma that has failed previous systemic treatment. This indication is conditionally approved based on the objective response rate results of a single-arm clinical trial. Full approval of this indication will depend on whether the ongoing confirmatory randomized controlled clinical trials can confirm the long-term clinical benefit for patients with advanced melanoma.
Dosage and Administration:
This product must be used under the guidance of a physician with experience in tumor treatment. The recommended dose of Toripalimab is 3 mg/kg, intravenously infused once every 2 weeks until disease progression or unacceptable toxicity occurs. Atypical reactions have been observed in patients treated with this product (e.g., temporary enlargement of the tumor or the appearance of new small lesions within the first few months of treatment, followed by tumor shrinkage). If the patient’s clinical symptoms are stable or continuously alleviated, even if there is preliminary evidence of disease progression, based on the judgment of overall clinical benefit, continued treatment with this product may be considered until disease progression is confirmed. Depending on the safety and tolerability of individual patients, it may be necessary to suspend administration or permanently discontinue use. Increasing or decreasing the dose is not recommended. Please see Table 1 for guidance on suspending or permanently discontinuing administration. For detailed guidance on the management of immune-related adverse reactions, please see [Precautions]. Special Populations Hepatic Impairment The safety and efficacy of this product in patients with moderate or severe hepatic impairment have not been established, and it is not recommended for patients with moderate or severe hepatic impairment. Patients with mild hepatic impairment should use this product with caution under the guidance of a physician. If used, no dose adjustment is required. Renal Impairment The safety and efficacy of this product in patients with moderate or severe renal impairment have not been established, and it is not recommended for patients with moderate or severe renal impairment. Patients with mild renal impairment should use this product with caution under the guidance of a physician. If used, no dose adjustment is required. Pediatric Population The safety and efficacy of this product in children and adolescents under 18 years of age have not been established, and no relevant data are available. Elderly Population Currently, there is limited data on its use in the elderly (65 years and above). It is recommended to use it with caution under the guidance of a physician. If used, no dose adjustment is required.
Adverse Reactions:
This instruction manual describes the approximate incidence of adverse reactions observed in clinical trials that are judged to be potentially related to Teplizumab. Because clinical trials are conducted in different patient populations and under various conditions, the incidence of adverse reactions observed in different clinical trials cannot be directly compared and may not reflect the actual incidence in clinical practice. Safety Summary The safety summary of monotherapy of this product comes from 8 single-arm, open-label, single/multicenter clinical studies. A total of 598 patients were included, including advanced melanoma (n=191), nasopharyngeal carcinoma (n=135), esophageal cancer (n=65), gastric cancer (n=63), head and neck squamous cell carcinoma (n=34), non-small cell lung cancer (n=33), breast cancer (n=20), lymphoma (n=24), soft tissue sarcoma (n=12), urothelial carcinoma (n=9), renal cancer (n=6), pancreatic cancer (n=2) and other types of tumors (n=4). The dosage of this product is 0.3mg/kg (n=3), 1mg/kg (n=39), 3mg/kg (n=522), 10mg/kg (n=31), 240mg (n=3). Among them, in the 3mg/kg group, 132 patients (25.3%) were exposed for ≥6 months, and 67 patients (12.8%) were exposed for ≥12 months. The incidence of adverse reactions of all levels in monotherapy with this product was 93.8%, and the adverse reactions with an incidence of ≥10% were anemia, increased ALT, fatigue, increased AST, rash, fever, increased blood thyroid stimulating hormone, decreased white blood cell count, cough, itching, hypothyroidism, decreased appetite, increased blood sugar and increased blood bilirubin. Most adverse reactions were mild to moderate (grade 1-2). The incidence of grade 3 and above adverse reactions was 29.4%, and the incidence of ≥1% was anemia, hyponatremia, infectious pneumonia, increased amylase, increased lipase, increased ALT, fatigue, increased AST and thrombocytopenia. Adverse reactions in clinical studies Melanoma HMO-JS001-II-CRP-01 is an open, multicenter, single-arm, Phase II clinical study that enrolled patients with inoperable or metastatic melanoma who had previously failed systemic treatment. A total of 128 patients received treatment with 3 mg/kg of toripalimab every 2 weeks until disease progression or unacceptable toxicity. The median exposure time of patients was 4.33 months (range: 1 day to 19.7 months). Among patients treated with this product, the incidence of all adverse reactions was 97.7%, and the adverse reactions with an incidence of ≥10% were rash, skin depigmentation, itching, anemia, fatigue, hypothyroidism, decreased appetite, fever, and cough. Among them, the incidence of grade 3 and above adverse reactions was 28.9%, and the incidence of grade 3 and above adverse reactions with an incidence of ≥1% were hypertriglyceridemia, anemia, hypertension, liver damage, and thrombocytopenia. The incidence of drug-related serious adverse events (SAEs) was 11.7%, and the incidence of drug-related SAEs with an incidence of ≥1% were pancreatitis, liver damage, upper gastrointestinal bleeding, and thrombocytopenia. 15.6% of patients permanently discontinued the drug due to adverse reactions, with an incidence of ≥1% for increased ALT, increased blood creatine phosphokinase, increased AST, pancreatitis, thrombocytopenia, increased amylase, increased lipase, liver injury, and upper gastrointestinal bleeding. 7.0% of patients suspended the drug due to adverse reactions, with an incidence of ≥1% for increased ALT, hypertriglyceridemia, and rash. In this study, adverse reactions (incidence ≥5%) in patients treated with this product alone are summarized in Table 2, and laboratory abnormalities (incidence ≥10%) are summarized in Table 3. For detailed descriptions of the images, please refer to Table 3 of the drug instructions for laboratory abnormalities of all grades with an incidence of ≥10% in the HMO-JS001-II-CRP-01 study (N=128)*: For detailed descriptions of the images, please refer to the drug instructions for specific adverse reaction descriptions The following information is derived from the summary safety information of 598 subjects in 8 single-arm studies of this product. For detailed management guidelines for the following immune-related adverse reactions, please refer to [Precautions]. Immune-related pneumonitis: Eleven patients (1.8%) developed immune-related pneumonitis in patients treated with this product, including 2 patients (0.3%) with grade 1, 3 patients (0.5%) with grade 2, 4 patients (0.7%) with grade 3, and 2 patients (0.3%) with grade 5. The median time to onset was 2.1 months (range 0.6-7.7 months), and the median duration was 8.3 months (range 0.4-15.1+ months). Seven patients (1.2%) permanently discontinued this product due to immune-related pneumonitis, and two patients (0.3%) needed to suspend this product. Among them, 9 patients (81.8%) received corticosteroid treatment, with a median starting dose of 60.0 mg (range 10.0-100.0 mg) of prednisone and a median duration of 22.0 days (range 3.0-42.0 days), of which 7 patients (63.6%) received high-dose (≥40 mg prednisone equivalent) corticosteroid treatment. Among the 11 patients, 1 (9.1%) had complete remission, with a remission time of 1.4 months, and 8 (72.7%) patients had stable conditions. Immune-related diarrhea and colitis Among the patients treated with this product, 1 (0.2%) patient had grade 3 immune-related diarrhea, and no colitis occurred. The time to onset was 12.6 months, and the duration was 0.1 month. The patient’s condition has been relieved. Immune-related hepatitis Among the patients treated with this product, 21 (3.5%) patients had immune-related hepatitis, including 2 (0.3%) grade 2, 12 (2.0%) grade 3, 6 (1.0%) grade 4, and 1 (0.2%) grade 5. The median time to onset was 1.4 months (range 0.1-8.4 months), and the median duration was 1.6 months (range 0.1-15.3+ months). Ten patients (1.7%) needed to permanently discontinue this product, and 4 patients (0.7%) needed to suspend this product. Two patients (9.5%) received corticosteroid treatment, with a median starting dose of 62.5 mg (range 62.5-80.0 mg) of prednisone and a median duration of 10.0 days (range 8.0-10.0 days), all of which were high-dose (≥40 mg prednisone equivalent) corticosteroid treatment. Eight patients (38.1%) had a remission, with a median remission time of 0.9 months (range 0.2-5.3 months). Immune-related nephritis Five patients (0.8%) developed immune-related nephritis in patients treated with this product, including one (0.2%) with grade 2, three (0.5%) with grade 3, and one (0.2%) with grade 4. There were no grade 5 cases. The median time to onset was 3.0 months (range 0.7-10.6 months), and the median duration was 0.7 months (range 0.1-14.8+ months). The disease was relieved in 3 patients (60.0%), with a median remission time of 0.3 months (range 0.1-1.0 months). Immune-related endocrine diseases Hypothyroidism Among the patients treated with this product, a total of 77 patients (12.9%) developed hypothyroidism, including 42 patients (7.0%) with grade 1 and 35 patients (5.9%) with grade 2, and no cases of grade 3 or above. The median time to the onset of hypothyroidism was 2.8 months (range 0.3-14.0 months), and the median duration was 7.2 months (range 0.3-17.4+ months). 2 patients (0.3%) needed to permanently discontinue this product, and 1 patient (0.2%) needed to suspend this product. 45 patients (58.4%) received thyroid hormone replacement therapy, of which 36 patients (46.8%) needed to continue to receive thyroid hormone replacement therapy. 20 patients (26.0%) had a remission, with a median remission time of 1.5 months (range 0.3-8.3 months). Hyperthyroidism Among the patients treated with this product, a total of 29 patients (4.8%) developed hyperthyroidism, including 24 patients (4.0%) with grade 1, 5 patients (0.8%) with grade 2, and no cases of grade 3 or above. The median time to the onset of hyperthyroidism was 1.8 months (range 0.5-17.6 months), and the median duration was 1.4 months (range 0.4-21.4+ months). No patient needed to permanently stop using this product, and 2 patients (0.3%) needed to suspend this product. Among them, 2 patients (6.9%) continued to receive antithyroid drugs. 19 patients (65.5%) had a remission, with a remission time of 1.3 months (range 0.4-7.5 months). Hyperglycemia and type 1 diabetes Among patients treated with this product, 17 patients (2.8%) developed hyperglycemia or type 1 diabetes, including 13 patients (2.2%) with grade 1, 1 patient (0.2%) with grade 2, 2 patients (0.3%) with grade 3, and 1 patient (0.2%) with grade 4. There were no cases of diabetic ketoacidosis or grade 5. The median time to the onset of hyperglycemia or type 1 diabetes was 2.1 months (range 0.4-11.8 months), and the median duration was 1.1 months (range 0.4-18.3+ months). One patient (0.2%) required permanent discontinuation of this product, and one patient (0.2%) required suspension of this product. Nine patients (52.9%) had a remission, with a median remission time of 0.5 months (range 0.4-4.6 months). Adrenal insufficiency Among patients treated with this product, 2 patients (0.3%) developed immune-related adrenal insufficiency, both of which were grade 2. The median time to adrenal insufficiency was 4.2 months (range 1.9-6.5 months), and the median duration was 11.3 months (range 6.8-11.3+ months). One patient (0.2%) required permanent discontinuation of this product, and no patient required suspension of this product. Both patients received corticosteroids, with a median starting dose of prednisone of 33.3 mg (range 7.5-33.3 mg) and a median duration of 19.0 days (range 19.0-19.0 days). The condition of both patients was stable. Hypophysitis Grade 3 immune-related hypophysitis occurred in one patient (0.2%) treated with this product. The time to onset was 7.4 months, and the duration was 3.7+ months. The patient permanently discontinued treatment with this product and continued to receive 5 mg prednisone replacement therapy, and his condition was stable. Immune-related skin adverse reactions Among patients treated with this product, 19 patients (3.2%) had immune-related skin adverse reactions, including 13 cases (2.2%) of grade 1, 6 cases (1.0%) of grade 2, and no cases of grade 3 or above. The median time to onset was 1.3 months (range 0.1-10.5 months), and the median duration was 4.9 months (range 0.1-20.7+ months). One patient (0.2%) needed to permanently stop using this product, and 3 patients (0.5%) needed to suspend this product. 18 patients (94.7%) received corticosteroid treatment, mainly topical, with a median starting dose of prednisone of 33.3 mg (range 4.0-33.3 mg), and a median duration of administration of 18.0 days (range 1.0-312.0 days). No patient received high-dose (≥40 mg prednisone equivalent) corticosteroid treatment. Eleven patients (57.9%) had a remission, with a median duration of remission of 2.0 months (range 0.1-5.6 months). Other immune-related adverse reactions Thrombocytopenia Among patients treated with this product, 6 patients (1.0%) developed immune-related thrombocytopenia, including 1 patient (0.2%) with grade 3, 4 patients (0.7%) with grade 4, and 1 patient (0.2%) with grade 5. The median time to onset was 0.6 months (range 0.1-6.4 months), and the median duration was 0.3 months (range 0.1-16.1+ months). Three patients (0.5%) required permanent discontinuation of this product, and one patient (0.2%) required suspension of this product. No patient received corticosteroid treatment. Four patients (66.7%) had a remission, with a median duration of remission of 0.3 months (range 0.1-1.3 months). Pancreatitis Among patients treated with this product, 16 patients (2.7%) developed immune-related pancreatitis/elevated amylase/elevated lipase. Among them, 1 patient (0.2%) had grade 2, 11 patients (1.8%) had grade 3, and 4 patients (0.7%) had grade 4. Among them, 12 patients (2.0%) had asymptomatic elevated amylase/elevated lipase, including 1 patient (0.2%) with grade ≥4. The median time to onset was 1.0 month (range 0.4-7.4 months), and the median duration was 1.1 months (range 0.1-17.6+ months). Four patients (0.7%) needed to permanently discontinue this product, and three patients (0.5%) needed to suspend this product. No patient was treated with corticosteroids. Eight patients (50.0%) had a remission, with a median remission time of 0.7 months (range 0.1-1.7 months). Other immune-related adverse reactions with low incidence (≤1%) in patients exposed to this product: 1 case of grade 2 iritis, 1 case of grade 3 uveitis, and 1 case of grade 2 polymyositis.
Share:
Products
Our offers
Health Classification
Let us work together to protect precious health